Denton A. Cooley, MD, and the Texas Heart Institute
James J. Livesay, MD, Gregory N. Messner, DO, and William K. Vaughn, PhD
- PMID: 16107099
- PMCID: PMC1163455
The history of the treatment of aortic aneurysm is remarkable and worthy of study because it parallels most of the great advances in medicine over the past 2,000 years. In the 2nd century AD, Antyllus provided the first record of the cause and treatment of aneurysm. Osler described him as one of the most daring and accomplished surgeons in history, due to his early proximal and distal ligation of aneurysms.1 In 1555, Vesalius was first to diagnose an abdominal aortic aneurysm.2 Lancisi published a comprehensive text on the pathology of aneurysms, complete with case studies, in 1728.2 The British surgeons William and John Hunter performed a number of ligations of peripheral aneurysms, while Astley Cooper was first to ligate the abdominal aorta for a ruptured iliac aneurysm in 1817.1 A major advance in the treatment of aneurysms came in 1888 with Rudolf Matas’s concept of endoaneurysmorrhaphy.3 After obtaining proximal and distal control, he obliterated the aneurysmal sac, oversewing collaterals yet preserving a lumen for blood flow (Fig. 1).
Fig. 1 Technique for restorative aneurysmorrhaphy developed by Rudolph Matas. Note that a lumen is preserved and the aneurysm is plicated. Reprinted from Ann Surg, 1903.3
Cooley’s First Aneurysm
The modern treatment of aortic aneurysm can be traced directly from advances in congenital heart surgery in the 1940s.1 Blalock’s development of vascular anastomosis techniques for palliation of congenital heart defects and Gross’s repair of coarctation of the aorta by end-to-end anastomosis, and later by homograft replacement, served as catalysts to surgical repair of aortic aneurysm. From the ranks of an outstanding house staff assembled by Blalock at Johns Hopkins University came a very talented young surgeon from Houston (Fig. 2). Denton A. Cooley’s remarkable career would parallel the advances in aortic surgery over the next 50 years. Cooley’s first experience with aneurysm surgery has been reported.1,4 As a resident in 1949, Cooley was assisting Grant Ward in removing an infected metallic prosthesis from the sternum when bleeding ensued from an underlying pseudoaneurysm of the ascending aorta. Ward controlled the bleeding with his left hand but was unable to use his right hand because of a chronic partial paralysis. Ward informed Cooley that he would have to repair the lesion, which he did using a pectoralis muscle patch. The patient survived. A 2nd patient presented in 1950 with a large pseudoaneurysm of the right subclavian artery, 3 months after a coarctation repair by Blalock. Because Blalock was out of town, Cooley repaired the aneurysm by ligating the subclavian artery proximally and distally, via a trapdoor sternotomy. He achieved a 2nd successful outcome.
Fig. 2 Surgical house staff of Johns Hopkins University, 1950. Alfred Blalock is shown in the center of the photo with chief resident Denton Cooley on his left. Reprinted from Tex Heart Inst J, 2001.4
Cooley joined the faculty at Baylor College of Medicine under Michael DeBakey in 1951. Shortly after his arrival, Cooley was presented with a 48-year-old man who had a saccular aneurysm of the aortic arch. During the operation, Cooley placed a clamp across the neck of the aneurysm, removed the aneurysm, and oversewed it. The procedure was termed a tangential excision and lateral aortorrhaphy when Cooley presented his first 6 cases in 1951.5 Numerous milestones were surpassed in Houston in only 5 short years. The number of pioneering surgical procedures reported by Cooley and DeBakey is staggering. Although Dubost was first to replace an abdominal aneurysm with an aortic homograft in 1951, Cooley and DeBakey followed several months later in the United States.6 They reported successful repair of a thoracic aneurysm in 1952 and resection of aneurysm of the distal aortic arch in 1953.5,7 They described replacement of a thoracic aneurysm with a homograft in 19558 and total excision of the aortic arch, also in 1955.9 Methods for treatment of aortic dissection were presented the same year.10 In 1956, Cooley reported the first homograft replacement of the entire ascending aorta, using cardiopulmonary bypass.11
The pioneering spirit of Cooley can be appreciated by reading the early report of his first attempt at total resection of the aortic arch.9 The patient was a 49-year-old man with a large syphilitic aneurysm of the aortic arch and a 2nd aneurysm of the descending aorta. The patient was operated in June 1955, 1 year before the pump oxygenator was available in Houston. A temporary shunt was constructed with a 14-mm Ivalon tube to provide circulation to the carotids and distal aorta (Fig. 3). Surface cooling (91°F) was used for cerebral protection. Total excision of the aortic arch and replacement with a custom-made Ivalon prosthesis was performed. After the reconstruction, the temporary shunt was removed. The procedure went smoothly; however, the right carotid shunt became occluded for 8 minutes before flow could be restored. The patient sustained a stroke and later died. In the discussion of the paper, Cooley recommended the use of heparin in the future and felt that hypothermia had been partially protective.
Fig. 3 Total excision of the aortic arch for treatment of aneurysm. A temporary shunt was constructed prior to resection of the aneurysm and subsequent reconstruction of the arch with an Ivalon prosthesis. Reprinted with permission from J Am Coll Surg, formerly Surg Gynecol & Obstet 1955;101:667–72,9 figures 2, ,3,3, 4, and 5.
Texas Heart Institute Contributions
The Texas Heart Institute was founded in 1963 by Cooley to promote research, stimulate education, and advance patient care in cardiovascular disease. A number of advances in aortic surgery have been made by the faculty since that time. Improved methods of repair have been applied to aneurysms of the ascending aorta and aortic root. In 1961, Cooley coined the term annuloaortic ectasia to describe the aneurysmal dilatation of the aortic root that often occurs in patients with Marfan syndrome.12 Modifications of the Bentall and Cabrol procedure and supracoronary replacement have been reported.13 Reports from the Texas Heart Institute have described improved methods of treating aortic dissection, and of treating sinus of Valsalva aneurysm and fistula.14,15
For aneurysms involving the aortic arch, Cooley contributed a method of classification that is helpful because it distinguishes aneurysms by location, extent, and preferred technique for repair.2 Since protection of the brain is a primary consideration for repair of aneurysms involving the aortic arch, Cooley was either the first to describe or to make significant improvements in the methods currently used for cerebral protection. Through his vast clinical experience, he has reported the use of bypass shunts, surface hypothermia, cerebral perfusion, and deep hypothermia with circulatory arrest for cerebral protection.16 Anesthetic techniques using high-dose barbiturates were found to afford a level of protection.17 Ott reported the use of deep hypothermia (18°C) and circulatory arrest in 1978.18 Recognizing the associated problems of bleeding and organ dysfunction with deep hypothermia, Cooley modified his approach using moderate hypothermia (24°C), shortened periods of circulatory arrest, and improved graft preparation.19 Using these methods, Livesay reported a decline in surgical mortality from 50% to 10% for repair of aortic arch aneurysm.20 Innovative surgical techniques such as open aortic anastomosis, avoidance of arterial clamping in aortic dissection, hemi-arch repair, and modification of the elephant trunk technique have simplified the procedure.2,14,19,20 Recognizing the serious problem of bleeding in association with deep hypothermia, Cooley in 1981 developed a method to prepare woven Dacron grafts.21 The grafts were soaked in the patient’s own plasma and then autoclaved to seal the interstices of the graft with coagulated protein. This innovative concept had a dramatic effect in reducing postoperative bleeding and mortality,19 and it led to the development of today’s commercially manufactured grafts.
For aneurysms of the descending thoracic aorta, one of the greatest concerns is the avoidance of spinal cord injury. Most of the methods for spinal protection used today were first described by Cooley. He proposed hypothermia for spinal protection in 1954 and later studied hypothermic perfusion in 1987.22,23 He first demonstrated the protective effect of cerebral spinal fluid drainage in 1962.24 He described the use of distal perfusion for descending thoracic aneurysms in 1968.25 In 1985, Livesay compared the results of surgery, with and without distal perfusion, in 360 patients. The risk of paraplegia was related to the location and extent of the aneurysm, advanced age, emergency status, and cross-clamp time longer than 30 minutes.26 Perfusion circuits were not found to decrease the risk of paraplegia or renal failure. Kay demonstrated that applying the aortic cross-clamp proximal to the left subclavian or even the left carotid artery for aneurysms of the distal aortic arch did not increase the risk of complications.27 Reul reported that aortic dissections of the descending thoracic aorta could be managed successfully by surgical repair.28
In Cooley’s classic report on the treatment of ruptured abdominal aneurysms, prompt control of hemorrhage was obtained by aortic clamping of the supraceliac abdominal aorta.6 Recognizing the need for improved vascular grafts, Cooley helped develop a double velour Dacron graft in 1978.29 This graft was found to enable improved tissue in-growth and endothelial coverage. Reul demonstrated the importance of coronary revascularization in reducing the risk of subsequent abdominal aortic repair.30 He reported a contemporary series of infrarenal abdominal aneurysm repairs with a mortality rate of 1.6%.31 In patients with infected aortic grafts or aorto-enteric fistula, Walker showed, contrary to conventional teaching, that improved outcomes could be achieved by “in situ” replacement with a new graft and long-term antibiotic coverage.32 Duncan presented a comprehensive review of the THI experience with aortitis and mycotic aneurysm.33 Hallman contributed to a report on inflammatory aneurysms.34
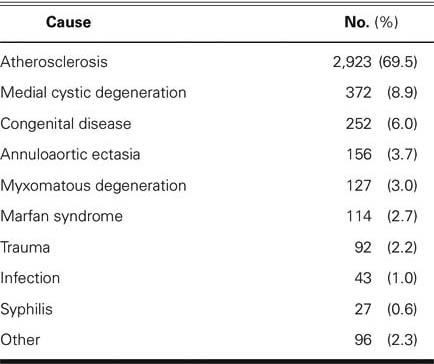
Over the past 5 decades, Cooley and the THI surgical staff have contributed 247 peer-reviewed manuscripts on aortic surgery and related topics. In addition, Cooley has written 3 textbooks on the subject. The modern approach of endoaneurysmorrhaphy, as adapted from Matas, has been applied in 8,459 procedures at the Texas Heart Institute over the past half century. The anatomic locations of the aneurysms are shown in Table I. The age distribution of patients is given in Table II. The cause is presented in Table III.
TABLE I. Texas Heart Institute Experience with Aortic Aneurysms, 1953–2004

TABLE II. Age of Patients with Aortic Aneurysms
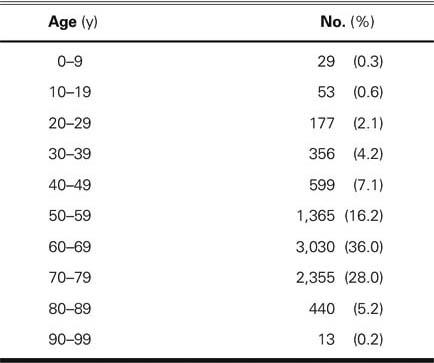
TABLE III. Cause of Aortic Aneurysm
Closing Comment
Progress has been made in the treatment of aortic aneurysms over the past 50 years. Improvements in patient care, surgical techniques, and visceral organ protection have resulted in reduced operative risks and enhanced long-term outcomes. The career and accomplishments of Denton A. Cooley have contributed immensely to our modern treatment of aortic aneurysms. For his unparalleled contributions to the treatment of this life-threatening disease, Denton Cooley has earned the undying respect and gratitude of his colleagues, students, fellow surgeons, and countless thousands of patients worldwide afflicted by aortic aneurysms.
Footnotes
Address for reprints: James J. Livesay, MD, Department of Cardiovascular Surgery, Texas Heart Institute, MC 3-258, 1101 Bates Street, Suite P-514, Houston, TX 77030. E-mail: ude.cmt.iht.traeh@yasevilj
Presented at the 14th International Meeting of the Denton A. Cooley Cardiovascular Surgical Society, 6–10 October 2004, Houston, Texas
References
Articles from Texas Heart Institute Journal are provided here courtesy of Texas Heart Institute
Over the years, there have been significant milestones in the treatment of aortic aneurysm, transforming how this life-threatening condition is diagnosed and managed. An aortic aneurysm occurs when there is a weakened and bulging area in the wall of the aorta, the main blood vessel that carries oxygenated blood from the heart to the rest of the body. Left untreated, it can lead to rupture, which is often fatal. Fortunately, thanks to advances in medical technology, the treatment and management of aortic aneurysms have come a long way.
One of the earliest milestones in the treatment of aortic aneurysms was the development of surgical repair methods, with open surgery being the standard approach for many years. In the 1990s, the introduction of endovascular aneurysm repair (EVAR) marked a pivotal shift. This minimally invasive technique allowed surgeons to repair aneurysms using small incisions and a catheter, reducing recovery times and complications for patients.
Another major milestone was the development of better imaging techniques, such as high-resolution CT scans and MRIs, which have significantly improved the ability to detect aortic aneurysms early, allowing for more timely intervention. Furthermore, advances in biomaterials have led to the creation of more durable stent grafts that are used in endovascular procedures, improving long-term outcomes.
Today, the treatment of aortic aneurysms continues to evolve with ongoing research focused on improving patient outcomes, including genetic therapies and new drugs aimed at preventing aneurysm growth. As medical science progresses, the future holds the potential for even more innovative solutions to manage this potentially deadly condition. These milestones in the treatment of aortic aneurysm not only highlight the progress made but also offer hope for patients facing this serious health risk.