Igor D. Gregoric, MD, Michael T. Nolen, MD, Jus Ksela, MD, Linda B. Chandler, RN, Gregory N. Messner, DO, Roberto D. Cervera, MD, Frank W. Smart, MD, Reynolds M. Delgado, III, MD, and O. H. Frazier, MD
- PMID: 16392237
- PMCID: PMC1336728
Abstract
A 57-year-old man, who had received a heart transplant 14 years earlier, underwent coronary artery bypass grafting and transmyocardial laser revascularization for left main, left anterior descending, and circumflex coronary artery disease. The procedures were performed through a left thoracotomy incision without cardiopulmonary bypass. Because the patient was of the Jehovah’s Witness faith, no blood or blood products were transfused.
Keywords: Angina pectoris, blood loss, surgical/prevention & control, cardiac surgical procedures/methods, coronary artery bypass, off-pump, heart transplantation, human, Jehovah’s Witnesses, lasers, male, middle-aged, myocardial revascularization/methods, religion and medicine, reoperation, risk factors
Jehovah’s Witness patients may refuse to undergo transfusion of blood or blood products, even when faced with a life-threatening hemorrhage. Over the years, special techniques have been developed for performing major cardiac operations, including heart transplantation, in these patients.1–7 Nevertheless, because of the heightened risk of severe bleeding, only a few institutions will accept such patients for reoperation. We describe the case of a Jehovah’s Witness patient who, 14 years after receiving a heart transplant, developed coronary occlusive disease in the transplanted heart. We discuss surgical techniques and other factors to be considered in patients such as this.
Case Report
In May 1989, a 43-year-old man with severe dilated cardiomyopathy underwent heart transplantation at our institution. Because he was of the Jehovah’s Witness faith, the operation was performed without blood transfusion. His postoperative course was uneventful, and immunosuppression was accomplished with cyclosporine, prednisone, and azathioprine. The patient did well until October 2002, when a follow-up examination showed, for the 1st time, mild coronary artery occlusive disease in the transplanted heart. In May 2003, left-sided heart catheterization revealed severe stenosis of the left main (80%), left anterior descending (LAD) (70%), and circumflex (80%) coronary arteries. Initially, the patient was treated conservatively, but he continued to have angina. Two months later, adenosine magnetic resonance imaging showed reversible subendocardial hypoperfusion involving the anterolateral to inferolateral wall of the mid left ventricle. The ventricle was otherwise normal in size and function, with an ejection fraction of 0.58. The patient, then 57 years old, was advised to undergo coronary artery bypass grafting (CABG) and transmyocardial laser revascularization (TMLR). In July 2003, these procedures were performed through a left thoracotomy incision without cardiopulmonary bypass or the transfusion of blood or blood products.
Surgical Technique
Techniques for performing off-pump CABG and TMLR via a left thoracotomy have been described elsewhere.8 In our patient, after general endotracheal anesthesia was administered, a transesophageal echocardiography transducer was introduced. The patient was positioned for a left anterolateral thoracotomy, and the chest was entered via the 5th intercostal space. The left internal mammary artery (LIMA) and left greater saphenous vein were harvested. Systemic heparin (2 mg/kg) was then administered. With a sutureless anastomotic device (Symmetry™ Bypass System Aortic Connector, St. Jude Medical; St. Paul, Minn), the saphenous vein graft was anastomosed to the descending thoracic aorta proximally and was brought through a small posterior pericardiotomy. A coronary stabilizer was then applied, and the vein graft was anastomosed distal to the obtuse marginal branch with running 6-0 polypropylene sutures. The LAD was then exposed and stabilized in a similar fashion. The LIMA was anastomosed to the LAD, end-to-side, with 7-0 polypropylene sutures. The effects of heparin were then reversed with protamine.
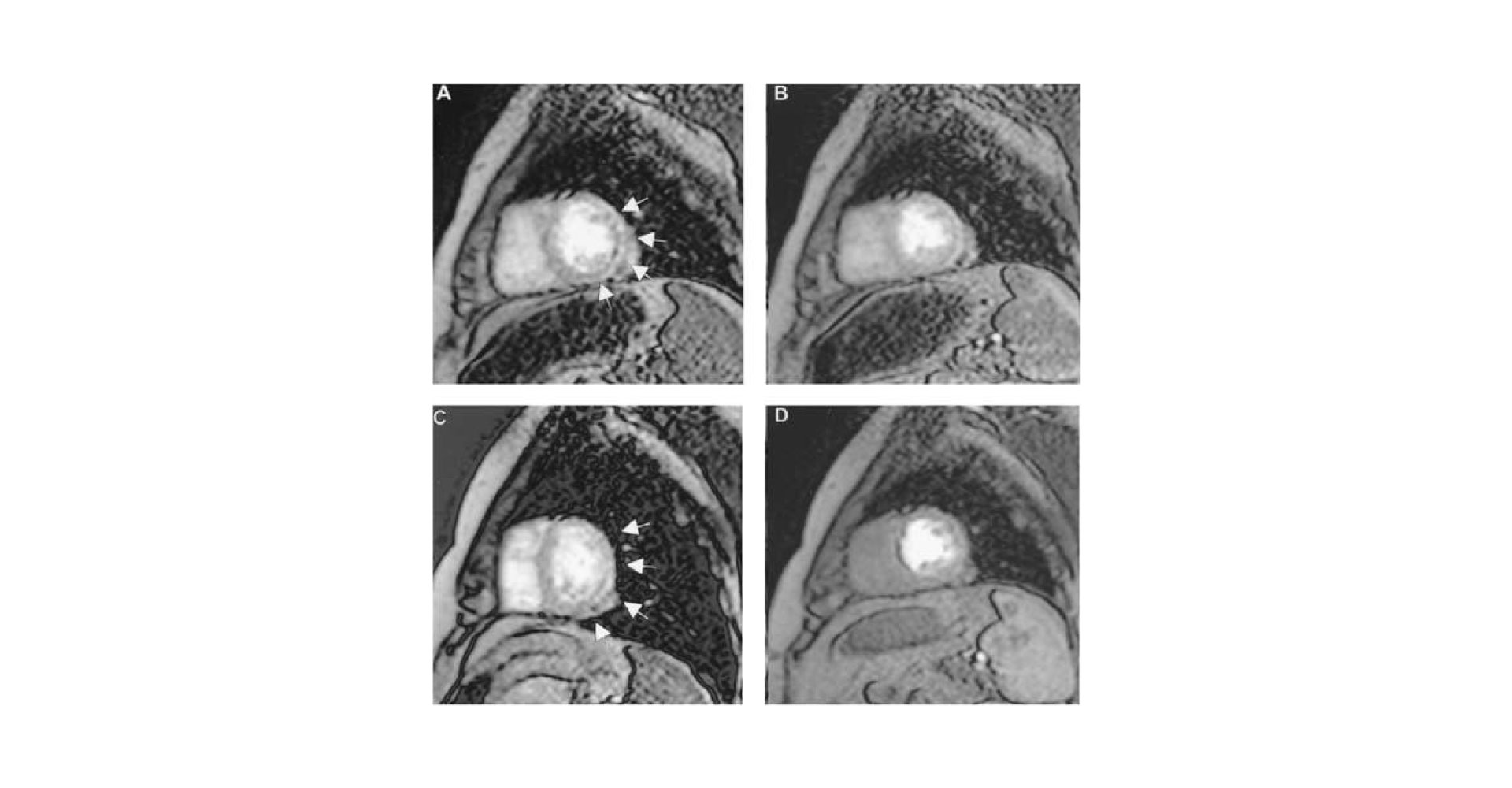
When complete hemostasis was achieved and the operative field was totally dry, TMLR was performed in the target areas of the left ventricle. Multiple transmural channels, each measuring about 1 mm in diameter, were created individually with a single pulse of a carbon dioxide laser (peak power, 850 W) in the posterolateral wall of the left ventricle. Transmural penetration by the laser was confirmed by transesophageal echocardiography. Bleeding from the channels was stopped with external pressure. The total amount of blood lost was approximately 300 cc. After satisfactory hemostasis was attained, the chest was closed. The patient was extubated 12 hours later and was discharged on the 5th postoperative day. In a 2-year telephone follow-up, the patient reported that he was free of cardiac symptoms including angina, shortness of breath, and physical restrictions (New York Heart Association functional class I). Figure 1, a comparison of preoperative and postoperative magnetic resonance images, shows improved endocardial perfusion after TMLR.
Fig. 1 Magnetic resonance images obtained during stress (A) and at rest (B) reveal preoperative endocardial hypoperfusion (black area indicated by arrows) consistent with clinically important ischemia. After transmyocardial laser revascularization, significantly improved perfusion of the endocardium is seen during stress (C) and at rest (D).
Discussion
The effect of CABG or angioplasty on long-term survival in heart transplant patients is still controversial. In our patient, despite optimal medical management, the disease progressed during a 10-month period, causing chest pain. Severe left main coronary artery disease, with extension to the LAD and circumflex artery, precluded coronary stenting.
Most patients who undergo reoperative cardiac surgery receive a perioperative blood transfusion. Because of their faith-based refusal to accept blood or blood products, Jehovah’s Witness patients who undergo cardiac reoperation present a unique challenge. Notwithstanding, such operations have been reported.5–7 Careful planning with a multidisciplinary approach is crucial to the treatment of these patients, especially heart transplant recipients undergoing surgical revascularization for severe coronary artery disease.
In our patient, the preoperative magnetic resonance image showed hypoperfusion of the anterolateral and inferolateral segments of the left ventricle. We considered doing a repeat sternotomy but decided that the lowest-risk option would be to perform CABG with a LIMA graft to the LAD and a saphenous vein graft to the obtuse marginal artery, followed by adjunctive TMLR through a left thoracotomy to provide neoangiogenesis. Our previous results with this approach had been encouraging.8 To maximize blood conservation during surgery and avoid hemodilution in this patient, we used an off-pump CABG technique. We performed the aortic graft anastomosis with a Symmetry Bypass System Aortic Connector and without a partial occlusion clamp. This simplified the technique and minimized the risk of aortic injury. To prevent major blood loss, we performed TMLR at the end of CABG, after the effects of heparinization were reversed. This is not our standard approach; the TMLR is usually done before CABG. Because of the severity of the left main disease in this patient, however, revascularization was performed first. During the procedure, a cell saver was used for blood conservation. The patient recovered uneventfully and was discharged on the 5th day after surgery.
Conclusion
Complex and even repeated cardiac operations may be performed successfully in Jehovah’s Witnesses. The treatment challenges presented by this patient population can be overcome—with use of modern technology, an appropriate surgical approach, and effective strategies for blood conservation—thus honoring the patient’s faith-based mandate while providing the highest standard of surgical care. This case proves that, with careful preoperative planning, complicated coronary artery disease can be safely managed in a Jehovah’s Witness heart transplant recipient.
Footnotes
Address for reprints: Igor D. Gregoric, MD, Texas Heart Institute, MC 2-114A, P.O. Box 20345, Houston TX 77225-0345
E-mail: ude.cmt.iht.traeh@cirogergi
References
Articles from Texas Heart Institute Journal are provided here courtesy of Texas Heart Institute
Posttransplant off-pump coronary bypass is a vital procedure for heart transplant patients who experience coronary artery disease (CAD) after their transplant. In heart transplant recipients, CAD can develop as a result of graft dysfunction, rejection, or other complications, potentially threatening the success of the transplant. This surgical technique offers a solution by providing coronary artery bypass without the need for a heart-lung machine, allowing the heart to continue beating during surgery.
The use of off-pump coronary bypass has shown to be particularly beneficial in posttransplant patients, as it reduces the risk of complications associated with traditional coronary bypass surgery, which often requires cardiopulmonary bypass. By bypassing the use of a heart-lung machine, surgeons can reduce the stress placed on the transplanted heart, promoting quicker recovery and minimizing postoperative complications such as arrhythmias and infections.
In posttransplant off-pump coronary bypass, the procedure is performed while the heart is still functioning, and the surgeon uses specialized instruments to bypass blocked arteries, restoring proper blood flow to the heart muscle. This method helps improve the long-term function of the transplanted heart by addressing coronary artery disease without compromising the transplant.
Recent advancements in surgical techniques and technology have further improved the outcomes of off-pump coronary bypass in posttransplant patients. The reduced risk of complications, shorter recovery times, and improved heart function make this technique an essential part of post-transplant care. As more research is conducted into the benefits of posttransplant off-pump coronary bypass, its role in enhancing the quality of life for heart transplant patients continues to grow. The procedure not only restores coronary circulation but also gives patients a better chance at long-term survival and improved heart health.